 Have you been diagnosed with a lumbar disc herniation and are considering surgery? Are you experiencing pain that seems to originate in the back and travels down the leg, calf, or even to the foot? If you’ve been led to believe that the only answer to this problem is the scalpel, please keep reading. There is another way. Ways, actually. The best way to treat lumbar disc pain, whether with or without sciatica, should be a custom-tailored plan tailored to your specific situation.
Have you been diagnosed with a lumbar disc herniation and are considering surgery? Are you experiencing pain that seems to originate in the back and travels down the leg, calf, or even to the foot? If you’ve been led to believe that the only answer to this problem is the scalpel, please keep reading. There is another way. Ways, actually. The best way to treat lumbar disc pain, whether with or without sciatica, should be a custom-tailored plan tailored to your specific situation.
And we have your plan. We’ll get into the specifics in a moment, but first, let’s review what we know about lumbar disc herniation.
First, it is incredibly common and not always painful. There is research suggesting that upward of 50% of people over the age of 20 have asymptomatic disc herniation. Disc herniation is often painless and is associated with the aging process. Sometimes, though, they can become painful and lead to other issues such as sciatica, which clinically is called “lumbar radiculopathy.”
This happens when the soft nucleus of the disc extrudes through the harder, fibrous outer rings that usually contain the nucleus. These rings are called the annulus fibrosus. If the extruding nucleus exits in a way that makes contact with the nearby exiting nerve roots, the resulting nerve compression can cause pain that travels into the lower extremities.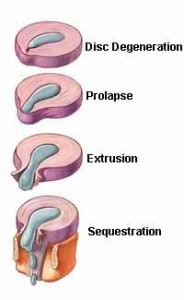
There are several treatment options available for this condition. Surgery should be the last option, as there are no guarantees that the procedure will be successful, and there are often complications to surgery that last a lifetime. The associated costs are far greater than those of non-surgical management, and post-surgical rehabilitation takes longer than the non-surgical protocols for resolving the issue in the first place.
One of the most critical components of treatment is obtaining an accurate diagnosis of the pain generator for the specific patient. As was just mentioned, it is highly possible to have a disc herniation and no symptoms. What this means is that even if you’ve had an MRI that shows a bulging disc, your symptoms may not be caused by it. There are several reasons people can experience radiating pain, including sciatica pain that is unrelated to the discs. It’s also true that some symptoms can be caused by more than one issue in the back at the same time.
Assuming that your pain is disc-derived, non-surgical treatments vary from one practitioner to another. Generally speaking, there are often movements/exercises that, when performed with repetition, can ease the symptoms and change the morphology of the disc. When this happens, the patient has identified what is called the “directional preference” for exercises, which should become the first line of defense against their condition.
These exercises are often referred to as “McKenzie exercises” after the late Robin McKenzie, who discovered, quite by accident, that the repetition of specific movements was helpful for patients with disc pain. These exercises are also called “end range loading” exercises. Physical therapists and some chiropractors most often use this protocol.
Another standard treatment for bulging/herniated discs is something called “spinal decompression.” This therapy typically involves a table on which the patient lies, while being harnessed at the hips. The table then uses mechanical traction to gently decompress the lumbar spine, creating a vacuum effect within the injured disc. This vacuum effect has been known to reduce the size of the disc bulge throughout several treatments.
Next up are stabilization exercises. These exercises increase the core’s stamina more than its strength. This is done intentionally, as research shows core stamina is more important to the protection of the lower back than sheer strength. Most of these exercises require no equipment and should be done daily. This treatment is often done by any practitioner who treats low back pain. Or at least that should be.
Another component of disc-derived low back pain that frankly is often forgotten about during evaluation in most clinics is myofascial pain. Fascia is the name of the connective tissue that covers all the muscles and allows them to slide smoothly over one another. Disc pain often leads to continuous muscle guarding that lasts for days or even weeks, and this guarding can derange the fascia, resulting in further pain. Treating this condition typically requires hands-on manual therapy, which competent massage therapists and some chiropractors often perform.
Finally, there are nutritional interventions for disc-specific low back pain. It is well known in the literature that the body will eventually resorb the disc material that extrudes beyond the annular ring. When a herniation occurs, enzymes known as Matrix Metalloproteinases (MMPs) start to work on consuming the nuclear material. The worse the disc herniation, the faster this process happens, which is ironic because the bigger extrusions are usually the ones most likely targeted for surgical intervention.
There are enzymes found in certain whole food supplements that mimic the action of MMPs, and can speed up the healing of the injured disc. Practitioners most likely to use this type of intervention include chiropractors, naturopaths, and some medical doctors.
If you’ve read this far, you’re probably wondering why we’re sharing all of this information and what exactly we do at Green Chiropractic for lumbar disc herniation. The answer is simple. We do all of it. Except better. Because there are even better versions of some of the treatments mentioned here, and since we custom-tailor a plan just for you, you’ll receive the best plan tailored to your needs.
Another important consideration is that not all diagnosticians are created equally. Dr. Green did an externship with one of the most well-known chiropractors in the country, Dr. Don Murphy. Dr. Murphy is the author of several textbooks on the evaluation and treatment of spine disorders and is on staff at Brown University, where he lectures medical students on low back pain. He is considered a master diagnostician, and Dr. Green spent several months with him watching patient evaluations. Dr. Green was also the recipient of the Clinical Excellence Award in his graduating class at chiropractic college, which further exemplifies his pursuit of excellence in the field.
In short, the people you choose to work with matter. Not everyone does equally well in their educational pursuits. Dr. Green graduated at the top of his class, won a prestigious award, participated in one of the most sought-after externships in the country, and, according to the statistics, has some of the best clinical outcomes.
But what if you have an exceptionally bad disc and have the imaging to prove it? What if all the material that is supposed to be inside the disc now lies on the outside? Can these treatment protocols still work? Let’s look at a case study:
 This 26-year-old patient entered our office with extreme back pain and sciatica. He couldn’t stand upright without further exacerbating his symptoms. We began treating him 3x a week. After one week, the patient was doing a little better but was unsure of the diagnosis and requested an MRI. Here’s a picture of the image (left).
This 26-year-old patient entered our office with extreme back pain and sciatica. He couldn’t stand upright without further exacerbating his symptoms. We began treating him 3x a week. After one week, the patient was doing a little better but was unsure of the diagnosis and requested an MRI. Here’s a picture of the image (left).
The red circle indicates a severe herniation at L5/S1, one of the most common areas for this condition to occur.
Now convinced, the patient went “all in” on the treatment. We added the enzyme product and end-range loading exercises to be performed both in the office and at home, along with spinal decompression.
Within two weeks, his pain was under control well enough for him to return to his physically demanding job.
A week later, the patient was out of town and got into a fight(!) at a bar. When he returned to the clinic, he had scratches on his arm that prompted the doctor to ask about them. The patient described the fight, and that although he went to the ground with the other guy, his back never bothered him.
All of this for a patient who would have been on the operating table had he presented with this MRI finding at a surgeon’s clinic.
Total treatment time varies from patient to patient, but the results generally come quickly. Most patients who follow through on the home exercise program find that, within a few days, they are feeling much better, and by the end of the month, there are often no symptoms left to treat. What’s more, the home exercise program and end-range loading exercises become a first line of defense against any future bouts of disc pain. Patients often report that the education they received, along with the exercises, helped them stay calm in the presence of a flare-up. A big part of controlling back pain is understanding it, and we do everything we can to help you on that front.
Our final thought for you is this: when one only has a hammer, one tends to see every problem as a nail. The surgeon’s hammer is the scalpel, which is the most invasive tool available. It just makes sense to go to the place using the most tools and the least invasive hammer. We’re happy you’ve found your way to this page.
To discuss pricing and scheduling, call us at 832-203-5884